Unraveling ALS: Breakthrough Discoveries That Could Change Lives
Amyotrophic Lateral Sclerosis (ALS), commonly known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that profoundly impacts the lives of those diagnosed and their families. Characterized by the degeneration of motor neurons in the brain and spinal cord, ALS leads to a debilitating loss of muscle control, ultimately resulting in paralysis. With an average life expectancy of just two to five years post-diagnosis, the urgency for advancements in understanding and treating this devastating disease has never been greater.
Recent Discoveries in ALS Research
Recent studies have identified over 40 genes associated with ALS, significantly enhancing our understanding of its genetic underpinnings. This genetic insight opens new avenues for potential treatment targets, offering hope for more effective therapies. Notably, mutations in the SOD1 gene are linked to approximately 15% of familial ALS cases, highlighting the role of genetics in disease manifestation.
Dr. Michael Ward, an NIH neurologist, emphasizes the importance of these discoveries: “We have never been in a better position from a research standpoint to begin to understand what causes ALS and how to reverse that.” This sentiment reflects the optimism among researchers as they delve deeper into the molecular mechanisms that contribute to ALS development.
Breakthrough Treatments on the Horizon
The U.S. Food and Drug Administration (FDA) has recently granted accelerated approval for QALSODY (tofersen), a groundbreaking treatment aimed at reducing neurofilament levels—a key marker of neurodegeneration in ALS patients. This approval marks a significant milestone in ALS treatment, as it addresses one of the critical aspects of the disease’s progression.
Clinical trials are currently underway for various other potential therapies, many of which show promise in slowing disease progression or alleviating symptoms. The collaborative efforts of researchers, clinicians, and advocacy groups are pivotal in driving these advancements forward.
The Role of Inflammation and Immune Response
Researchers are increasingly exploring the role of inflammation and the immune response in ALS. Understanding how these factors contribute to the disease could open new therapeutic avenues. Recent studies suggest that targeting the interaction between TDP-43 and RGNEF proteins may offer a novel strategy to mitigate ALS progression.
As Dr. Rita Sattler, an ALS expert at the Barrow Neurological Institute, explains, “We have these proteins lacking in the nucleus, and they don’t do what they’re supposed to be doing in the nucleus. At the same time, we have them clumping outside the nucleus.” This mismanagement of TDP-43 is a common pathological feature in ALS, leading to toxic aggregates that contribute to neuronal death.
Advancements in Technology and Data Analysis
Advancements in artificial intelligence and machine learning are being harnessed to analyze large datasets related to ALS, potentially identifying new biomarkers and treatment strategies. These technologies can help researchers track disease progression and evaluate treatment efficacy more effectively.
For instance, researchers are investigating biomarkers such as neurofilament light chain and TDP-43 levels to monitor ALS progression. The identification of reliable biomarkers is crucial for assessing the effectiveness of new therapies and improving patient outcomes.
The Impact of Public Awareness and Funding
The Ice Bucket Challenge significantly raised awareness and funding for ALS research, leading to accelerated discoveries and advancements in treatment options. Philanthropic efforts, such as those from the Temerty Foundation, continue to play a vital role in supporting ALS research and facilitating breakthroughs in treatment development.
Continued advocacy and funding are essential to sustain momentum in ALS research. The collaborative efforts of researchers, clinicians, and advocacy groups are crucial in driving forward the search for effective therapies and improving the lives of those affected by ALS.
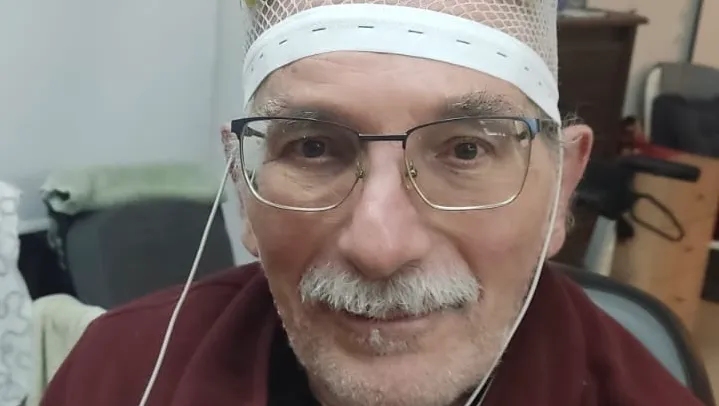
The Importance of Early Diagnosis
Early diagnosis of ALS is critical, as timely intervention can help manage symptoms and improve patient outcomes. However, it can take up to 18 months to receive a definitive diagnosis. This delay can have serious consequences, as the disease progresses rapidly, making early detection and intervention vital.
Health care providers typically perform a physical exam and review medical history to diagnose ALS. While there is no definitive blood test for ALS, neurologists assess muscle strength and reflexes to monitor disease progression. The development of computer-based tools to detect speech changes may also enhance early diagnosis efforts.
Supportive Care and Quality of Life
Supportive care and multidisciplinary approaches are crucial for managing ALS symptoms and improving the quality of life for patients and their families. Speech and communication difficulties are common in ALS patients, prompting the development of advanced speech-generating technologies and brain-computer interfaces.
Dr. Jordan Green, a speech-language pathologist, emphasizes the importance of early intervention: “It’s really important to see a speech pathologist very early on in the disease.” This proactive approach can help patients learn to use assistive devices before losing the ability to communicate.
Conclusion
The journey to unraveling ALS is filled with challenges, yet the




Leave a Comment